Detector Novedoso de Latidos Atípicos para el Diagnóstico Temprano de Enfermedades Cardíacas Basado en la Representación de Latidos Apilados de un Electrocardiograma de 12 Derivadas
DOI:
https://doi.org/10.17488/RMIB.44.4.6Palabras clave:
detección de latidos atípicos, enfermedades cardiovasculares en etapa temprana, análisis asistido por computadora de ECG, medicina preventiva, representación de latidos apilados de ECGResumen
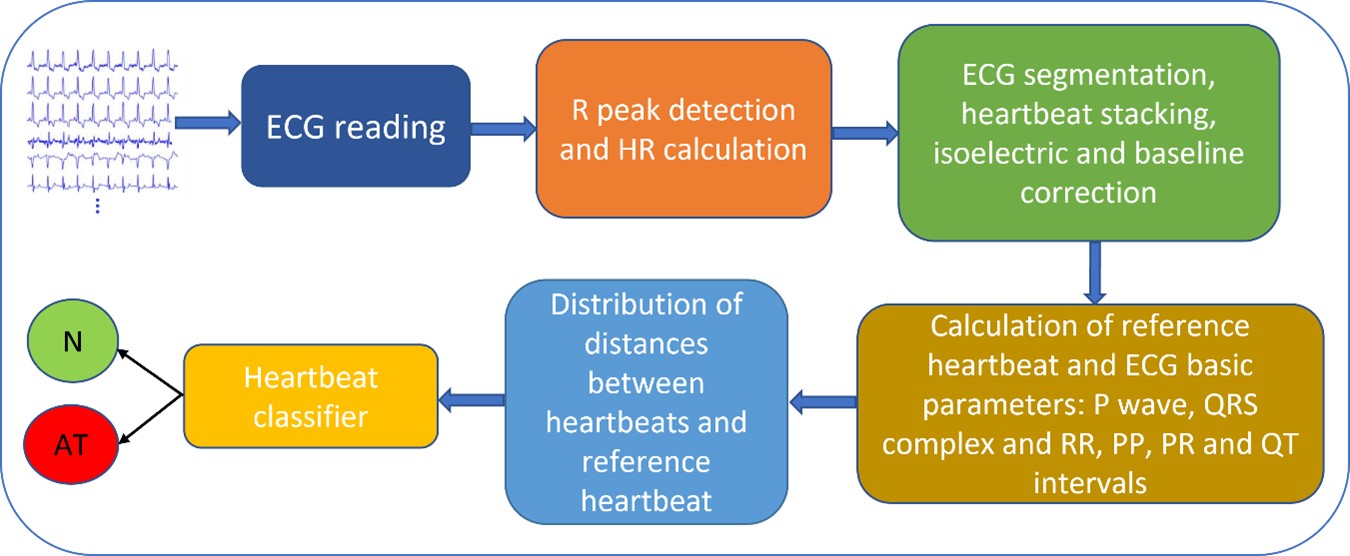
Desarrollamos y presentamos una serie de algoritmos que muestran un electrocardiograma (ECG) de larga duración en forma compacta de latidos apilados, extrayendo y visualizando características básicas y facilitando el tedioso y lento proceso de análisis de ECG para cardiólogos. El sistema experto basado sobre esta representación provee detección de latidos cardíacos atípicos, precursores de enfermedades cardiovasculares (ECV) y su ubicación en cada uno de las 12 derivadas. Este sistema se probó exhaustivamente con dos bases de datos públicas, base de datos de arritmias del MIT-BIH y China Physiological Signal Challenge (CPSC2018), lo que demostró su rápido procesamiento de ECG y alta eficiencia en la detección de anomalías en la morfología de los latidos. En particular, las pruebas en la base de datos CPSC2018 revelaron que el conjunto de ECG marcados como normales contiene una cantidad considerable de derivadas con latidos atípicos. El sistema se utiliza como clasificador en dos clases, latidos normales y atípicos, siendo estos últimos indicadores de enfermedades cardiovasculares (ECV). Se considera potencialmente útil para estudios de rutina en grupos con alto riesgo de ECV en etapas tempranas, como herramienta de medicina preventiva en el área de salud pública. El sistema permite la intervención del cardiólogo en etapas intermedias del análisis del ECG para corroborar el diagnóstico en casos ambiguos.
Descargas
Citas
C. K. Jha & M. H. Kolekar, “Empirical Mode Decomposition and Wavelet Transform Based ECG Data Compression Scheme,” IRBM, vol. 42, no. 1, pp. 65–72, Feb. 2021, doi: https://doi.org/10.1016/j.irbm.2020.05.008
B. Mohamed, A. Issam, A. Mohamed, & B. Abdellatif, “ECG Image Classification in Real time based on the Haar-like Features and Artificial Neural Networks,” Procedia Comput. Sci., vol. 73, pp. 32–39, 2015, doi: https://doi.org/10.1016/j.procs.2015.12.045
I. Güler & E. D. Übeyli, “ECG beat classifier designed by combined neural network model,” Pattern Recognit., vol. 38, no. 2, pp. 199–208, Feb. 2005, doi: https://doi.org/10.1016/j.patcog.2004.06.009
L.-H. Wang, Y.-T. Yu, W. Liu, L. Xu, et al., “Three-Heartbeat Multilead ECG Recognition Method for Arrhythmia Classification,” IEEE Access, vol. 10, pp. 44046-44061, Apr. 2022, doi: https://doi.org/10.1109/ACCESS.2022.3169893
Z. Dokur & T. Ölmez, “ECG beat classification by a novel hybrid neural network,” Comput. Methods Programs Biomed., vol. 66, no. 2–3, pp. 167-181, Sep. 2001, doi: https://doi.org/10.1016/S0169-2607(00)00133-4
J.-S. Wang, W.-C. Chiang, Y.-L. Hsu, Y.-T. C. Yang, “ECG arrhythmia classification using a probabilistic neural network with a feature reduction method,” Neurocomputing, vol. 116, pp. 38-45, Sep. 2013, doi: https://doi.org/10.1016/j.neucom.2011.10.045
S. M. Anwar, M. Gul, M. Majid, M. Alnowami, “Arrhythmia Classification of ECG Signals Using Hybrid Features,” Comput. Math. Methods Med., vol. 2018, art. no. 1380348, 2018, doi: https://doi.org/10.1155/2018/1380348
F. A. Elhaj, N. Salim, A. R. Harris, T. T. Swee, T. Ahmed, “Arrhythmia recognition and classification using combined linear and nonlinear features of ECG signals,” Comput. Methods Programs Biomed., vol. 127, pp. 52-63, Apr. 2016, doi: https://doi.org/10.1016/j.cmpb.2015.12.024
M. K. Moridani, M. Abdi Zadeh, Z. Shahiazar Mazraeh, “An Efficient Automated Algorithm for Distinguishing Normal and Abnormal ECG Signal,” IRBM, vol. 40, no. 6, pp. 332-340, Dec. 2019, doi: https://doi.org/10.1016/j.irbm.2019.09.002
S. Sahoo, M. Mohanty, S. Behera, & S. Kumar Sabut, “ECG beat classification using empirical mode decomposition and mixture of features”, J. Med. Eng. Technol., vol. 41, no. 8, pp. 652-661, 2017, doi: https://doi.org/10.1080/03091902.2017.1394386
Ö. Yildirim, “A novel wavelet sequence based on deep bidirectional LSTM network model for ECG signal classification,” Comput. Biol. Med., vol. 96, pp. 189-202, May 2018, doi: https://doi.org/10.1016/j.compbiomed.2018.03.016
R. A. Alharbey, S. Alsubhi, K. Daqrouq, A. Alkhateeb, “The continuous wavelet transform using for natural ECG signal arrhythmias detection by statistical parameters,” Alex. Eng. J., vol. 61, no. 12, pp. 9243-9248, Dec. 2022, doi: https://doi.org/10.1016/j.aej.2022.03.016
J. Park & K. Kang, “PcHD: Personalized classification of heartbeat types using a decision tree,” Comput. Biol. Med., vol. 54, pp. 79-88, Nov. 2014, doi: https://doi.org/10.1016/j.compbiomed.2014.08.013
Y. Kutlu & D. Kuntalp, “A multi-stage automatic arrhythmia recognition and classification system,” Comput. Biol. Med., vol. 41, no. 1, pp. 37-45, Jan. 2011, doi: https://doi.org/10.1016/j.compbiomed.2010.11.003
J. Kim & H. Shin, “Simple and Robust Realtime QRS Detection Algorithm Based on Spatiotemporal Characteristic of the QRS Complex,” PLoS ONE, vol. 11, no. 3, art. no. e0150144, 2016, doi: https://doi.org/10.1371/journal.pone.0150144
N. Katsaouni, F. Aul, L. Krischker, S. Schmalhofer, L. Hedrich, M. H. Schulz, “Energy efficient convolutional neural networks for arrhythmia detection,” Array, vol. 13, art. no. 100127, 2022, doi: https://doi.org/10.1016/j.array.2022.100127
X. Yang, X. Zhang, M. Yang, L. Zhang, “12-Lead ECG arrhythmia classification using cascaded convolutional neural network and expert feature,” J. Electrocardiol., vol. 67, pp. 56-62, 2021, doi: https://doi.org/10.1016/j.jelectrocard.2021.04.016
S. G. Begum, E. Priyadarshi, S. Pratap, S. Kulshrestha, V. Singh, “Automated Detection of Abnormalities in ECG signals using Deep Neural Network,” Biomed. Eng. Adv., vol. 5, art. no. 100066, Jun. 2023, doi: https://doi.org/10.1016/j.bea.2022.100066
S. C. Mohonta, M. A. Motin, & D. K. Kumar, “Electrocardiogram Based Arrhythmia Classification Using Wavelet Transform with Deep Learning Model,” Sens. Bio-Sens. Res., vol. 37, 2022, doi: http://dx.doi.org/10.2139/ssrn.4088025
J. H. Abawajy, A.V. Kelarev, M. Chowdhury, “Multistage approach for clustering and classification of ECG data,” Comput. Methods Programs Biomed., vol. 112, no. 3, pp. 720-730, Dec. 2013, doi: https://doi.org/10.1016/j.cmpb.2013.08.002
W.-H. Jung & S.-G. Lee, “An Arrhythmia Classification Method in Utilizing the Weighted KNN and the Fitness Rule,” IRBM, vol. 38, no. 3, pp. 138-148, Jun. 2017, doi: https://doi.org/10.1016/j.irbm.2017.04.002
L. Lu, J. Yan, C. W. de Silva, “Feature selection for ECG signal processing using improved genetic algorithm and empirical mode decomposition,” Measurement, vol. 94, pp. 372-381, Dec. 2016, doi: https://doi.org/10.1016/j.measurement.2016.07.043
U. R. Acharya, P. Subbanna Bhat, S.S. Iyengar, A. Rao, Sumeet Dua, “Classification of heart rate data using artificial neural network and fuzzy equivalence relation,” Pattern Recognit., vol. 36, no. 1, pp. 61-68, Jan. 2003, doi: https://doi.org/10.1016/S0031-3203(02)00063-8
J. Rahul, M. Sora, L. D. Sharma, V. K. Bohat, “An improved cardiac arrhythmia classification using an RR interval-based approach,” Biocybern. Biomed. Eng., vol. 41, no. 2, pp. 656-666, 2021, doi: https://doi.org/10.1016/j.bbe.2021.04.004
R. Rohmantri & N. Surantha, “Arrhythmia Classification using 2D Convolutional Neural Network,” Int. J. Adv. Comput. Sci. Appl., vol. 11, no. 4, 2020, doi: http://dx.doi.org/10.14569/IJACSA.2020.0110427
S. L. Oh, E. Y. K. Ng, R. S. Tan, U. R. Acharya, Automated diagnosis of arrhythmia using combination of CNN and LSTM techniques with variable length heart beats, Comput. Biol. Med., vol. 102, pp. 278-287, Nov. 2018, doi: https://doi.org/10.1016/j.compbiomed.2018.06.002
B. Chen, D. M. Maslove, J. D. Curran, A. Hamilton, P. R. Laird, P. Mousavi, S. Sibley, “A deep learning model for the classification of atrial fibrillation in critically ill patients,” Intensive Care Med. Exp., vol. 11, art. no. 2, Jan. 2023, doi: https://doi.org/10.1186/s40635-022-00490-3
O. Yildirim, U. B. Baloglu, R.-S. Tan, E. J. Ciaccio, U. R. Acharya, “A new approach for arrhythmia classification using deep coded features and LSTM networks,” Comput. Methods Programs Biomed., vol. 176, pp. 121-133, Jul. 2019, doi: https://doi.org/10.1016/j.cmpb.2019.05.004
N. Du, Q. Cao, L. Yu, N. Liu, E. Zhong, Z. Liu, Y. Shen, K. Chen, Fm-ecg: A fine-grained multi-label framework for ecg image classification, Information Sciences 549 (2021) pp. 164–177, doi: https://doi.org/10.1016/j.ins.2020.10.014
A. Aranda Hernandez, P. Bonizzi, R. Peeters, J. Karel, “Continuous monitoring of acute myocardial infarction with a 3-Lead ECG system,” Biomed. Signal Process. Control, vol. 79, art. no. 104041, Jan. 2023, doi: https://doi.org/10.1016/j.bspc.2022.104041
G. B. Moody & R. G. Mark, “The impact of the MIT-BIH Arrhythmia Database,” IEEE Eng. Med. Biol. Mag., vol. 20, no. 3, pp. 45-50, 2001, doi: https://doi.org/10.1109/51.932724
F. Liu, C. Liu, L. Zhao, X. Zhang, et al., “An Open Access Database for Evaluating the Algorithms of Electrocardiogram Rhythm and Morphology Abnormality Detection,” J. Med. Imaging Health Inf., vol. 8, no. 7, pp. 1368–1373, 2018, doi: http://dx.doi.org/10.1166/jmihi.2018.2442
M. Bellamoli, F. Marin, L. Maritan, D. Prati, et al., “New-onset extreme right axis deviation in acute myocardial infarction: clinical characteristics and outcomes,” J. Electrocardiol., vol 60, pp. 60–66, 2020, doi: https://doi.org/10.1016/j.jelectrocard.2020.03.003
X. Gu, J. Hu, L. Zhang, J. Ding, F. Yan, “An Improved Method with High Anti-interference Ability for R Peak Detection in Wearable Devices,” IRBM, vol. 41, no. 3, pp. 172–183, Jun. 2020, doi: https://doi.org/10.1016/j.irbm.2020.01.002
C. Cakir, Y. Ceylan, O. Y. Akbal, R. Sarikaya, S. Barutcu, “Clinical characteristics and angiographic findings of non-st-elevation acute coronary syndrome patients admitted with normal electrocardiogram,” J. Electrocardiol., vol. 60, pp. 77–81, 2020, doi: https://doi.org/10.1016/j.jelectrocard.2020.03.002
N. Dugarte, E. Dugarte, N. Dugarte, Electrocardiografía de Alta Resolución Técnicas Aplicadas de Adquisición y Procesamiento, Argentina: Universidad Tecnológica Nacional (UTN-FRM), 2018.
R. Srivastva, A. Singh, Y. N. Singh, “PlexNet: A fast and robust ECG biometric system for human recognition,” Information Sciences, vol. 558, pp. 208-228, May 2021, doi: https://doi.org/10.1016/j.ins.2021.01.001
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Revista Mexicana de Ingenieria Biomedica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.
Una vez que el artículo es aceptado para su publicación en la RMIB, se les solicitará al autor principal o de correspondencia que revisen y firman las cartas de cesión de derechos correspondientes para llevar a cabo la autorización para la publicación del artículo. En dicho documento se autoriza a la RMIB a publicar, en cualquier medio sin limitaciones y sin ningún costo. Los autores pueden reutilizar partes del artículo en otros documentos y reproducir parte o la totalidad para su uso personal siempre que se haga referencia bibliográfica al RMIB. No obstante, todo tipo de publicación fuera de las publicaciones académicas del autor correspondiente o para otro tipo de trabajos derivados y publicados necesitaran de un permiso escrito de la RMIB.