A Review on the Advances of Biocompatible Materials and Their Processing Via Additive Manufacturing for Tissue Engineering Applications
DOI:
https://doi.org/10.17488/RMIB.44.3.2Keywords:
biomaterials, bioprinting, regenerative medicine, tissue engineeringAbstract
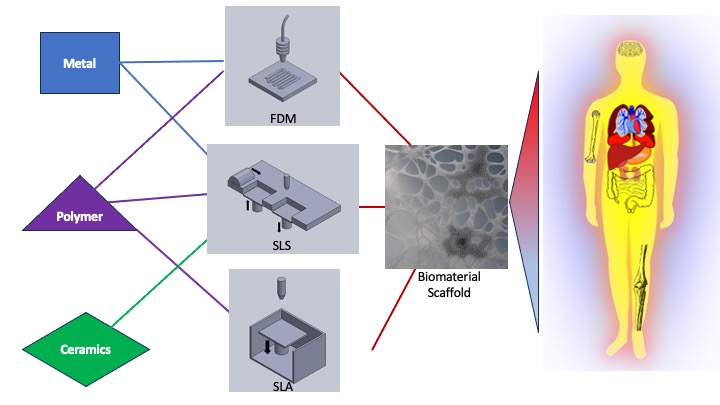
About two decades ago, medicine experienced a revolutionary approach, driven by technological development in manufacturing techniques and scientific advances in the medical and life sciences, the field took on the challenge of regenerating tissue and organs damaged by disease, trauma, or hereditary issues, incorporating additive manufacturing as one of its strategies. Since its inception, regenerative medicine has developed techniques like tissue engineering, cellular therapy, medical devices, and artificial organs to provide wound healing and orthopedic applications. The incorporation of additive manufacturing allowed to recreate biologically appropriate environments for cell reproduction and growth that, eventually, lead to useful, regenerated tissue or organs. The objective of the present work is to review recent advances in the application of additive manufacturing techniques and ad hoc biomaterials in the field of regenerative medicine, to determine their impact in the development of new therapies for tissue engineering.
Downloads
References
A. Atala, “Engineering tissues, organs, and cells,” J. Tissue Eng. Regen. Med., vol. 1, no. 2, pp. 83-96, Mar. 2007, doi: https://doi.org/10.1002/term.18
P. Zarrintaj, F. Seidi, M. Youssefi Azarfam, M. Khodadadi Yazdi, et al., “Biopolymer-based composites for tissue engineering applications,” Compos. B: Eng., vol. 258, art. no. 110701, Jun. 2023, doi: https://doi.org/10.1016/j.compositesb.2023.110701
A. O. Mahmoud Salehi, S. Heidari Keshel, F. Sefat, and L. Tayebi, “Use of polycaprolactone in corneal tissue engineering: A review,” Mater. Today Commun., vol. 27, art. no. 102402, Jun. 2021, doi: http://dx.doi.org/10.1016/j.mtcomm.2021.102402
Y. Ikada, “Challenges in tissue engineering,” J. R. Soc. Interface, vol. 3, no. 10, pp. 589-601, Apr. 2006, doi: https://doi.org/10.1098/rsif.2006.0124
R. S. Katari, A. Peloso, and G. Orlando, “Tissue engineering,” Adv. Surg., vol. 48, no. 1, pp. 137-154, Sep. 2014, doi: https://doi.org/10.1016/j.yasu.2014.05.007
H. Taneja, S. M. Salodkar, A. S. Parmar, and S. Chaudhary, “Hydrogel based 3D printing: Bio ink for tissue engineering,” J. Mol. Liquids, vol. 3, art. no. 120390, Dec. 2022, doi: https://doi.org/10.1016/j.molliq.2022.120390
M. Srinivas, E.H.J.G. Aarntzen, J.W.M. Bulte, W.J. Oyen, A. Heerschap, I.J.M. de Vries, C.G. Figdor, “Imaging of cellular therapies,” Adv. Drug. Deliv. Rev., vol. 62, no. 11, pp. 1080-1093, Aug. 2010, doi: https://doi.org/10.1016/j.addr.2010.08.009
H. N. Chia and B. M. Wu, “Recent advances in 3D printing of biomaterials,” Biofabrication, vol. 9, art. no. 4, Mar. 2015, doi: https://doi.org/10.1186/s13036-015-0001-4
A. Banihashemian, S. Z. Benisi, S. Hosseinzadeh, and S. Shojaei, “Biomimetic biphasic scaffolds in osteochondral tissue engineering: Their composition, structure and consequences,” Acta Histochem., vol. 125, no. 3, art. no. 152023, Apr. 2023, doi: https://doi.org/10.1016/j.acthis.2023.152023
T. J. Keane and S. F. Badylak, “Biomaterials for tissue engineering applications,” Semin. Pediatr. Surg., vol. 23, no. 3, pp. 112-118, Jun. 2014, doi: https://doi.org/10.1053/j.sempedsurg.2014.06.010
J. Li, M. Chen, X. Fan, and H. Zhou, “Recent advances in bioprinting techniques: approaches, applications and future prospects,” J. Transl. Med., vol. 14, no. 1, art. no. 271, Sep. 2016, doi: https://doi.org/10.1186/s12967-016-1028-0
M. W. Naing, C. K. Chua, K. F. Leong, and Y Wang, “Fabrication of customized scaffolds using computer-aided design and rapid prototyping techniques,” Rapid Prototyp. J., vol. 11, no. 4, pp. 249-259, Sep. 2005, doi: https://doi.org/10.1108/13552540510612938
B. P. Chan and K. W. Leong, “Scaffolding in tissue engineering: general approaches and tissue-specific considerations,” Eur. Spine J., vol. 17, pp. 467-479, Nov. 2008, doi: https://doi.org/10.1007%2Fs00586-008-0745-3
S. K. Nandi, G. Fielding, D. Banerjee, A. Bandyopadhyay, S. Bose, “3D-printed b-TCP bone tissue engineering scaffolds: Effects of chemistry on in vivo biological properties in a rabbit tibia model,” J. Mater. Res., vol. 33, no. 14, pp. 1939-1947, Jul. 2018, doi: https://doi.org/10.1557%2Fjmr.2018.233
N. Beheshtizadeh, Y. Asgari, N. Nasiri, A. Farzin, M. Ghorbani, N. Lotfibakhshaiesh, and M. Azami, “A network analysis of angiogenesis/osteogenesis-related growth factors in bone tissue engineering based on in-vitro and in-vivo data: A systems biology approach,” Tissue Cell, vol. 72, art. no. 101553, Oct. 2021, doi: https://doi.org/10.1016/j.tice.2021.101553
W. Xu, J. Zhu, J. Hu, and L. Xiao, “Engineering the biomechanical microenvironment of chondrocytes towards articular cartilage tissue engineering,” Life Sci., vol. 309, art. no. 121043, Nov. 2022 doi: https://doi.org/10.1016/j.lfs.2022.121043
T. K. Dash and V. B. Konkimalla, “Poly-є-caprolactone based formulations for drug delivery and tissue engineering: A review,” J. Control. Release, vol. 158, no. 1, pp. 15-33, Feb. 2012, doi: https://doi.org/10.1016/j.jconrel.2011.09.064
S.-W. Mok, R. Nizak, S.-C. Fu, K.-W. K. Ho, L. Qin, D. B. F. Saris, K.-M. Chan, and J. Malda, “From the printer: Potential of three-dimensional printing for orthopedic applications,” J. Orthop. Translat., vol. 6, pp. 42-49, Jul. 2016, doi: https://doi.org/10.1016/j.jot.2016.04.003
I. Ozbolat and H. Gudapati, “A review on design for bioprinting,” Bioprinting, vol. 3-4, pp. 1-14, Sep.-Dec. 2016, doi: https://doi.org/10.1016/j.bprint.2016.11.001
S. M. Giannitelli, D. Accoto, M. Trombetta, and A. Rainer, “Current trends in the design of scaffolds for computer-aided tissue engineering,” Acta Biomater., vol. 10, no. 2, pp. 580-594, Feb. 2014, doi: https://doi.org/10.1016/j.actbio.2013.10.024
M. Adamkiewicz and B. Rubinsky, “Cryogenic 3D printing for tissue engineering,” Cryobiology, vol. 71, no. 3, pp. 518-521, Dec. 2015, doi: https://doi.org/10.1016/j.cryobiol.2015.10.152
A. V. Raut, A. Agrawal, A. Bagde, P. Fulzele, and Z. Q. Syed, “3-D Bioprinting in cartilage tissue engineering for bioinks-short review,” Mater. Today: Proc., vol. 80, part 3, pp. 1858-1861, 2023, doi: https://doi.org/10.1016/j.matpr.2021.05.625
S. Bose, D. Ke, H. Sahasrabudhe, and A. Bandyopadhyay, “Additive manufacturing of biomaterials,” Prog. Mater. Sci., vol. 93, pp. 45-111, Apr. 2018, doi: https://doi.org/10.1016%2Fj.pmatsci.2017.08.003
F. Pati, D.-H. Ha, J. Jang, H. H. Han, J.-W. Rhie, and D.-W. Cho, “Biomimetic 3D tissue printing for soft tissue regeneration,” Biomaterials, vol. 62, pp. 164-175, Sep. 2015, doi: http://doi.org/10.1016/j.biomaterials.2015.05.043
D. H. Rosenzweig, E. Carelli, T. Steffen, P. Jarzem, and L. Haglund, “3D-printed ABS and PLA Scaffolds for Cartilage and Nucleus Pulposus Tissue Regeneration," Int. J. Mol. Sci., vol. 16, no. 7, pp. 15118-15135, Jul. 2015, doi: https://doi.org/10.3390/ijms160715118
K. Elkhoury, M. Morsink, L. Sanchez-Gonzalez, C. Khan, A. Tamayol, and A. Arab-Tehrany, “Biofabrication of natural hydrogels for cardiac, neural, and bone Tissue engineering Applications,” Bioact. Mater., vol. 6, no. 11, pp. 3904-3923, Nov. 2021, doi: https://doi.org/10.1016/j.bioactmat.2021.03.040
C. Mandrycky, Z. Wang, K. Kim, and D.-H. Kim, “3D bioprinting for engineering complex tissues,” Biotechnol. Adv., vol. 34, no. 4, pp. 422-434, 2016, doi: https://doi.org/10.1016/j.biotechadv.2015.12.011
J. Z. Manapat, Q. Chen, P. Ye, and R. C. Advincula, “3D Printing of Polymer Nanocomposites via Stereolithography,” Macromol. Mater. Eng., vol. 302, no. 9, art. no. 1700184, Sep. 2017, doi: https://doi.org/10.1002/mame.201600553
Q. Chen and G. A. Thouas, “Metallic implant biomaterials,” Mater. Sci. Eng. R Rep., vol. 87, pp. 1-57, Jan. 2015, doi: https://doi.org/10.1016/j.mser.2014.10.001
M. Hospodiuk, M. Dey, D. Sosnoski, and I. T. Ozbolat, “The bioink: A comprehensive review on bioprintable materials,” Biotechnol. Adv., vol. 35, no. 2, pp. 217-239, Mar.-Apr. 2017, doi: https://doi.org/10.1016/j.biotechadv.2016.12.006
S. Rafieyan, E. Vasheghani-Farahani, N. Baheiraei, and H. Keshavarz, “MLATE: Machine learning for predicting cell behavior on cardiac tissue engineering scaffolds,” Comput. Biol. Med., vol. 158, art. no. 106804, May 2023, doi: https://doi.org/10.1016/j.compbiomed.2023.106804
M. D. Fahmy, H. E. Jazayeri, M. Razavi, R. Masri, and L. Tayebi, “Three-Dimensional Bioprinting Materials with Potential Application in Preprosthetic Surgery,” J. Prosthodont., vol. 25, no. 4, pp. 310-318, Jun. 2016, doi: https://doi.org/10.1111/jopr.12431
D. V. Abere, S. A. Ojo, M. B. Paredes-Epinosa, A. Hakami, “Derivation of composites of chitosan-nanoparticles from crustaceans source for nanomedicine: A mini review,” Biomed. Eng. Adv., vol. 4, art. no. 100058, Dec. 2022, doi: https://doi.org/10.1016/j.bea.2022.100058
I. T. Ozbolat, W. Peng, and V. Ozbolat, “Application areas of 3D bioprinting,” Drug Discov. Today, vol. 21, no. 8, pp. 1257-1271, Aug. 2016, doi: https://doi.org/10.1016/j.drudis.2016.04.006
A. Shapira, R. Feiner, and T. Dvir, “Composite biomaterial scaffolds for cardiac tissue engineering,” Int. Mater. Rev., vol. 61, no. 1, pp. 1-19, Jan. 2016, doi: https://doi.org/10.1179/1743280415Y.0000000012
I. T. Ozbolat and M. Hospodiuk, “Current advances and future perspectives in extrusion-based bioprinting,” Biomaterials, vol. 76, pp. 321-343, Jan. 2016, doi: https://doi.org/10.1016/j.biomaterials.2015.10.076
Y. Zou, L. Zhang, L. Yang, F. Zhu, M. Ding, F. Lin, Z. Wang, and Y. Li, “"Click" chemistry in polymeric scaffolds: Bioactive materials for tissue engineering,” J. Control. Release, vol. 273, pp. 160-179, Mar. 2018, doi: https://doi.org/10.1016/j.jconrel.2018.01.023
Q. Zhang, J. Zhou, P. Zhi, L. Liu, C. Liu, A. Fang, and Q. Zhang, “3D printing method for bone tissue engineering scaffold,” Med. Nov. Technol. Devices, vol. 17, art. no. 100205, Mar. 2023, doi: https://doi.org/10.1016/j.medntd.2022.100205
K. K. Moncal, D. N. Heo, K. P. Godzik, D. M. Sosnoski, et al., “3D printing of poly(ε-caprolactone)/poly(D,L-lactide-co-glycolide)/ hydroxyapatite composite constructs for bone tissue engineering,” J. Mater. Res., vol. 33, pp. 1972-1986, Jul. 2018, doi: https://doi.org/10.1557/jmr.2018.111
A. Bruyas, F. Lou, A. M. Stahl, M. Gardner, W. Maloney, S. Goodman, and Y. P. Yang, “Systematic characterization of 3D-printed PCL/b-TCP scaffolds for biomedical devices and bone tissue engineering: Influence of composition and porosity,” J. Mater. Res., vol. 33, pp. 1948-1959, Jul. 2018, doi: https://doi.org/10.1557/jmr.2018.112
L. Dong, S.-J. Wang, X.-R. Zhao, Y.-F. Zhu, and J.-K. Yu, “3D-printed Poly(ϵ-caprolactone) Scaffold Integrated with Cell-laden Chitosan Hydrogels for Bone Tissue Engineering,” Sci. Rep., vol. 7, art. no. 13412, Oct. 2017, doi: https://doi.org/10.1038/s41598-017-13838-7
M. C. Araque-Monrós, A. Vidaurre, L. Gil-Santos, S. Gironés Bernabé, M. Monleón-Pradas, and J. Más-Estellés, “Study of the degradation of a new PLA braided biomaterial in buffer phosphate saline, basic and acid media, intended for the regeneration of tendons and ligaments,” Polym. Degrad. Stab., vol. 98, no. 9, pp. 1563-1570, Sep. 2013, doi: https://doi.org/10.1016/j.polymdegradstab.2013.06.031
F. Habibzadeh, S. M. Sadraei, R. Mansoori, N. P. S. Chauhan, and G. Sargazi, “Nanomaterials supported by polymers for tissue engineering applications: A review,” Heliyon, vol. 8, no. 12, art. no. E12193, Dec. 2022, doi: https://doi.org/10.1016/j.heliyon.2022.e12193
S. Rupnik, S. Buwalda, S. Dejean, A. Bethry, X. Garric, J. Coudane, and B. Nottelet, “Redox Reducible and Hydrolytically Degradable PEG–PLA Elastomers as Biomaterial for Temporary Drug-Eluting Medical Devices,” Macromol. Biosci., vol. 16, no. 12, pp. 1792-1802, Dec. 2016, doi: https://doi.org/10.1002/mabi.201600132
M. Mesa, L. Sierra, J. Patarin, and J.-L. Guth, “Morphology and porosity characteristics control of SBA-16 mesoporous silica. Effect of the triblock surfactant Pluronic F127 degradation during the synthesis,” Solid State Sci., vol. 7, no. 8, pp. 990-997, Aug. 2005, doi: https://doi.org/10.1016/j.solidstatesciences.2005.04.006
H. Taneja, S. M. Salodkar, A. S. Parmar, and S. Chaudhary, “Hydrogel based 3D printing: Bio ink for tissue engineering,” J. Mol. Liq., vol. 367, art. no. 120390, Dec. 2022, doi: https://doi.org/10.1016/j.molliq.2022.120390
R. Najafi, H. Chahsetareh, M. Pezeshki-Modaress, M. Aleemardani, et al., “Alginate sulfate/ECM composite hydrogel containing electrospun nanofiber with encapsulated human adipose-derived stem cells for cartilage tissue engineering,” Int. J. Biol. Macromol., vol. 238, art. no. 124098, May 2023, doi: https://doi.org/10.1016/j.ijbiomac.2023.124098
J. Yang, Y. S. Zhang, K. Yue, and A. Khademhosseini, “Cell-laden hydrogels for osteochondral and cartilage tissue engineering,” Acta Biomater., vol. 57, pp. 1-25, Jul. 2017, doi: https://doi.org/10.1016/j.actbio.2017.01.036
G. Gao, J. H. Lee, J. Jang, D. H. Lee, et al., “Tissue Engineered Bio-Blood-Vessels Constructed Using a Tissue-Specific Bioink and 3D Coaxial Cell Printing Technique: A Novel Therapy for Ischemic Disease,” Adv. Funct. Mater., vol. 27, no. 33, art. no. 1700798, Sep. 2017, doi: https://doi.org/10.1002/adfm.201700798
T. Distler and A. R. Boccaccini, “3D printing of electrically conductive hydrogels for tissue engineering and biosensors – A review,” Acta Biomater., vol. 101, pp. 1-13, Jan. 2020, doi: https://doi.org/10.1016/j.actbio.2019.08.044
J. Huang, “Desing and Development of Ceramics and Glasses,” in Biology and Engineering of Stem Cell Niches, A. Vishwakarma, J. M. Karp, Eds., 1st ed. San Diego, CA, United States: Academic Press, 2017, ch. 20, pp. 315-329.
Y. Wang, W. Zhang, and Q. Yao, “Copper-based biomaterials for bone and cartilage tissue engineering,” J. Orthop. Translat., vol. 29, pp. 60-71, Jul. 2021, doi: https://doi.org/10.1016/j.jot.2021.03.003
S. V. Murphy, A. Atala, “3D bioprinting of tissues and organs,” Nat. Biotechnol., vol. 32, no. 8, pp. 773-784, Aug. 2014, doi: https://doi.org/10.1038/nbt.2958
H. Gudapati, M. Dey, and I. Ozbolat, “A comprehensive review on droplet-based bioprinting: Past, present and future,” Biomaterials, vol. 102, pp. 20-42, Sep. 2016, doi: https://doi.org/10.1016/j.biomaterials.2016.06.012
P. Datta, B. Ayan, and I. T. Ozbolat, “Bioprinting for vascular and vascularized tissue biofabrication,” Acta Biomater., vol. 51, pp. 1-20, Mar. 2017, doi: https://doi.org/10.1016/j.actbio.2017.01.035
P. Bajaj, R. M. Schweller, A. Khademhosseini, J. L. West, and R. Bashir, “3D Biofabrication Strategies for Tissue Engineering and Regenerative Medicine,” Annu. Rev. Biomed. Eng., vol. 16, pp. 247-276, Jul. 2014, doi: https://doi.org/10.1146/annurev-bioeng-071813-105155
J. Holländer, R. Hakala, J. Suominen, N. Moritz, J. Yliruusi, N. Sandler, “3D printed UV light cured polydimethylsiloxane devices for drug delivery,” Int. J. Pharm., vol. 544, no. 2, pp. 433-442, Jun. 2018, doi: https://doi.org/10.1016/j.ijpharm.2017.11.016
I. T. Ozbolat, H. Chen, and Y. Yu, “Development of ‘Multi-arm Bioprinter’ for hybrid biofabrication of tissue engineering constructs,” Robot Comput. Integr. Manuf., vol. 30, no. 3, pp. 295-304, Jun. 2014, doi: https://doi.org/10.1016/j.rcim.2013.10.005
H. W. Kang, S. J. Lee, I. K. Ko, C. Kengla, J. J. Yoo, A. Atala, “A 3D bioprinting system to produce human-scale tissue constructs with structural integrity,” Nat. Biotechnol., vol. 34, no. 3, pp. 312-319, Feb. 2016, doi: https://doi.org/10.1038/nbt.3413
H. Kweon, M. K. Yoo, I. K. Park, T. H. Kim, H. C. Lee, et al., “A novel degradable polycaprolactone networks for tissue engineering,” Biomaterials, vol. 24, no. 5, pp. 801-808, Feb. 2003, doi: https://doi.org/10.1016/s0142-9612(02)00370-8
K. Arai, S. Iwanaga, H. Toda, C. Genci, Y. Nishiyama, M. Nakamura, “Three-dimensional inkjet biofabrication based on designed images,” Biofabrication, vol. 3, art. no. 034113, Sep. 2011, doi: http://dx.doi.org/10.1088/1758-5082/3/3/034113
Published
How to Cite
Issue
Section
License
Copyright (c) 2023 Revista Mexicana de Ingenieria Biomedica

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Upon acceptance of an article in the RMIB, corresponding authors will be asked to fulfill and sign the copyright and the journal publishing agreement, which will allow the RMIB authorization to publish this document in any media without limitations and without any cost. Authors may reuse parts of the paper in other documents and reproduce part or all of it for their personal use as long as a bibliographic reference is made to the RMIB. However written permission of the Publisher is required for resale or distribution outside the corresponding author institution and for all other derivative works, including compilations and translations.