Neuromarcadores basados en Estadística de EEG en el Dominio Temporal y Frecuencial para Detectar Acufeno
DOI:
https://doi.org/10.17488/RMIB.44.3.1Palabras clave:
acúfeno, características en frecuencia, características en tiempo, diagnóstico clínico, neuromarcadores, pérdida auditivaResumen
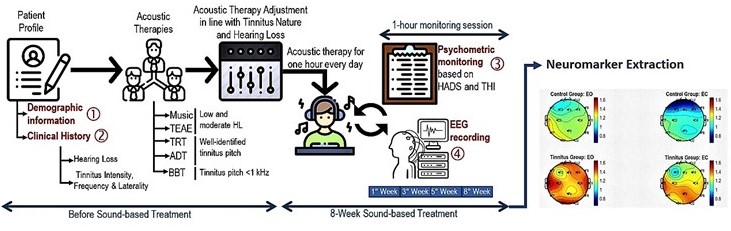
La detección y caracterización del acúfeno requiere un diagnóstico cuidadosamente elaborado debido principalmente a su naturaleza heterogénea. La presente investigación tiene como objetivo encontrar características en las señales electroencefalográficas (EEG) a partir del análisis del dominio del tiempo y frecuencia que podrían distinguir entre pacientes sanos y con acúfeno con diferentes niveles de pérdida auditiva. Para ello, se reclutaron 24 voluntarios y se dividieron por igual en cuatro grupos: 1) controles, 2) acúfeno bajo, 3) acúfeno medio y 4) acufeno alto. La actividad EEG se registró en reposo en dos condiciones: ojos cerrados y abiertos durante un minuto. El análisis de EEG se centró en anchos de banda delta y alfa. Para el dominio del tiempo, las características del EEG estimadas fueron la media, la desviación estándar, la curtosis, el pico máximo, la asimetría y la forma. Para el dominio de la frecuencia, las características de EEG obtenidas fueron media, asimetría, densidad espectral de potencia. La normalidad de los datos del EEG se evaluó mediante la prueba de Lilliefors y, como resultado, se aplicó la técnica no paramétrica del estadístico H de Kruskal-Wallis para probar la significación. Los resultados muestran que las características del EEG son más diferenciables entre los pacientes con acúfeno y los controles en el dominio de la frecuencia que en el dominio del tiempo. Las características del EEG de los pacientes con acúfeno con alta pérdida de audición son significativamente diferentes del resto de los grupos en la actividad de la banda de alfa cuando se calculan la forma y la asimetría.
Descargas
Citas
B. Hackenberg, K. O’Brien, J. Döge, K. J. Lackner, et al., “Tinnitus Prevalence in the Adult Population—Results from the Gutenberg Health Study,” Medicina, vol. 59, no. 3, art. no. 620, Mar. 2023, doi: https://doi.org/10.3390/medicina59030620
J. J. Eggermont, L. E. Roberts, “The neuroscience of tinnitus: understanding abnormal and normal auditory perception,” Front. Syst. Neurosci., vol. 6, art. no. 53, 2012, doi: https://doi.org/10.3389/fnsys.2012.00053
C. R. Cederroth, S. Gallus, D. A. Hall, T. Kleinjung, et al., “Towards an Understanding of Tinnitus Heterogeneity,” Front. Aging Neurosci., vol. 11, art. no. 53, 2019, doi: https://doi.org/10.3389/fnagi.2019.00053
W. Sedley, K. J. Friston, P. E. Gander, S. Kumar, T. D. Griffiths, “An Integrative Tinnitus Model Based on Sensory Precision,” Trends Neurosci., vol. 39, no. 12, pp. 799–812, Dec. 2016, doi: https://doi.org/10.1016/j.tins.2016.10.004
K. M. Reavis, V. S. Rothholtz, Q. Tang, J. A. Carroll, H. Djalilian, F.-G. Zeng, “Temporary Suppression of Tinnitus by Modulated Sounds,” J. Assoc. Res. Otolaryngol., vol. 13, no. 4, pp. 561–571, Apr. 2012, doi: https://doi.org/10.1007/s10162-012-0331-6
M. J. Guitton, “Tinnitus: pathology of synaptic plasticity at the cellular and system levels,” Front. Syst. Neurosci., vol. 6, art. no.12, 2012, doi: https://doi.org/10.3389/fnsys.2012.00012
S. Kalle, W. Schlee, R. C. Pryss, T. Probst, M. Reichert, B. Langguth, M. Spiliopoulou, “Review of Smart Services for Tinnitus Self-Help, Diagnostics and Treatments,” Front. Neurosci., vol. 12, art. no. 541, 2018, doi : https://doi.org/10.3389/fnins.2018.00541
C. W. Newman, S. A. Sandridge, G. P. Jacobson, “Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome,” J. Am. Acad. Audiol., vol. 9, no. 2, pp. 153–160, Apr. 1998. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/9564679/
I. Bjelland, A. A. Dahl, T. T. Haug, D. Neckelmann, “The validity of the Hospital Anxiety and Depression Scale: an updated literature review,” J. Psychosom. Res., vol.52, no. 2, pp. 69–77, Feb. 2002, doi: https://doi.org/10.1016/S0022-3999(01)00296-3
P. H. Wilson, J. Henry, M. Bowen, G. Haralambous, “Tinnitus reaction questionnaire: psychometric properties of a measure of distress associated with tinnitus,” J. Speech Hear Res., vol. 34, no. 1, pp. 197–201, Feb. 1991. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/2008074/
C. H. Bastien, A. Vallières, C. M. Morin, “Validation of the Insomnia Severity Index as an outcome measure for insomnia research,” Sleep Med., vol. 2, no. 4, pp. 297–307, Jul. 2001, doi: https://doi.org/10.1016/S1389-9457(00)00065-4
M. B. Frisch, “Quality-of-Life-Inventory,” in: Encyclopedia of Quality of Life and Well-Being Research, A. C. Michalos ed. Dordrecht: Springer, 2014, pp. 5374–5377, doi: https://doi.org/10.1007/978-94-007-0753-5_2371
A. Kadouri, E. Crruble, B. Falissard, “The improved Clinical Global Impression Scale (iCGI): development and validation in depression,” BMC Psychiatry, vol. 7, art. no.7, Feb. 2007, doi: https://doi.org/10.1186/1471-244X-7-7
C. Weise, M. Kleinstäuber, H. Hesser, V. Z. Westin, G. Andersson, “Acceptance of tinnitus: validation of the tinnitus acceptance questionnaire,” Cogn. Behav. Ther., vol. 42, no. 2, pp. 100–115, Apr. 2013, doi: https://doi.org/10.1080/16506073.2013.781670
A. T. Beck, R. A. Steer, G. Brown, Beck Depression Inventory–II (BDI-II), American Psychological Association, 1996, doi: https://psycnet.apa.org/doi/10.1037/t00742-000
J. A. Henry, S. Griest, E. Thielman, G. McMillan, C. Kaelin, K. F. Carlson, “Tinnitus Functional Index: Development, validation, outcomes research, and clinical application,” Hear. Res., vol. 334, pp. 58–64, Apr. 2016, doi: https://doi.org/10.1016/j.heares.2015.06.004
J. Horsman, W. Furlong, D. Feeny, G. Torrance, “The Health Utilities Index (HUI®): concepts, measurement properties and applications,” Health Qual Life Outcomes, vol. 1, art. no. 54, Oct. 2003, doi: https://doi.org/10.1186/1477-7525-1-54
M. Landgrebe, F. Zeman, M. Koller, Y. Eberl, et al., “The Tinnitus Research Initiative (TRI) database: a new approach for delineation of tinnitus subtypes and generation of predictors for treatment outcome,” BMC Med. Inform. Decis. Mak., vol. 10, art. no. 42, Aug. 2010, doi: https://doi.org/10.1186/1472-6947-10-42
R. F. F. Cima, G. Crombez, J. W. S. Vlaeyen, “Catastrophizing and Fear of Tinnitus Predict Quality of Life in Patients With Chronic Tinnitus,” Ear Hear., vol. 32, no. 5, pp. 634–641, Sep. 2011, doi: https://doi.org/10.1097/AUD.0b013e31821106dd
S. Levenstein, C. Prantera, V. Varvo, M. L. Scribano, E. Berto, C. Luzi, A. Andreoli, “Development of the Perceived Stress Questionnaire: A new tool for psychosomatic research,” J. Psychosom. Res., vol. 37, no. 1, pp. 19–32, Jan. 1993, doi: https://doi.org/10.1016/0022-3999(93)90120-5
M. Schecklmann, M. Landgrebe, B. Langguth, the TRI Database Study Group, “Phenotypic Characteristics of Hyperacusis in Tinnitus,” PLoS One, vol. 9, no. 1, art. no. e86944, Jan. 2014, doi: https://doi.org/10.1371/journal.pone.0086944
P. van de Heyning, G. Muehlmeier, T. Cox, G. Lisowska, H. Maier, K. Morawski, T. Meyer, “Efficacy and Safety of AM-101 in the Treatment of Acute Inner Ear Tinnitus—A Double-Blind, Randomized, Placebo-Controlled Phase II Study,” Otol. Neurotol., vol. 35, no. 4, pp. 589-597, Apr. 2014, doi: https://doi.org/10.1097/mao.0000000000000268
D. P. Spiegel, T. Linford, B. Thompson, M. A. Petoe, K. Kobayashi, C. M. Stinear, G. D. Searchfield, “Multisensory attention training for treatment of tinnitus,” Sci. Rep., vol. 5, art. no. 10802, 2015, doi: https://doi.org/10.1038/srep10802
E. Kara, K. Aydın, A. A. Akbulut, S. N. Karakol, et al., “Assessment of Hidden Hearing Loss in Normal Hearing Individuals with and Without Tinnitus,” J. Int. Adv. Otol., vol. 16, no. 1, art. no. 87, Apr. 2020, doi: https://doi.org/10.5152/iao.2020.7062
T. Langguth, B. Langguth, “Avenue for Future Tinnitus Treatments,” Otolaryngol. Clin. North Am., vol. 53, no. 4, pp. 667–683, Aug. 2020, doi: https://doi.org/10.1016/j.otc.2020.03.013
A. B. Elgoyhen, B. Langguth, D. De Ridder, S. Vanneste, “Tinnitus: perspectives from human neuroimaging,” Nat. Rev. Neurosci., vol. 16, no. 10, pp. 632–642, Oct. 2015, doi: https://doi.org/10.1038/nrn4003
H. Shojaeemend, H. Ayatollahi, “Automated Audiometry: A Review of the Implementation and Evaluation Methods,” Healthc. Inform. Res., vol. 24, no. 4, pp. 263-275, Oct. 2018, doi: https://doi.org/10.4258%2Fhir.2018.24.4.263
A. Parthasarathy, S. Romero Pinto, R. M. Lewis, W. Goedicke, D. B. Polley, “Data-driven segmentation of audiometric phenotypes across a large clinical cohort,” Sci. Rep., vol. 10, art. no. 6704, Apr. 2020, doi: https://doi.org/10.1038/s41598-020-63515-5
O. Ukaegbe, B. Ezeanolue, F. Orji, “The Influence of Tinnitus on the Audiometric Threshold of Sufferers,” Int. Arch. Otorhinolaryngol., vol. 20, no. 4, pp. 339–343, 2016, doi: https://doi.org/10.1055%2Fs-0035-1571271
R. Schaette, D. McAlpine, “Tinnitus with a Normal Audiogram: Physiological Evidence for Hidden Hearing Loss and Computational Model,” J. Neurosci., vol. 31, no. 38, pp. 13452–13457, Sep. 2011, doi: https://doi.org/10.1523/jneurosci.2156-11.2011
V. Vielsmeier, A. Lehner, J. Strutz, T. Steffens, et. al., “The Relevance of the High Frequency Audiometry in Tinnitus Patients with Normal Hearing in Conventional Pure-Tone Audiometry,” BioMed Res. Int., vol. 2015, art. no. 302515, 2015, doi: https://doi.org/10.1155/2015/302515
K. Ochi, T. Ohashi, M. Kenmochi, “Hearing Impairment and Tinnitus Pitch in Patients With Unilateral Tinnitus: Comparison of Sudden Hearing Loss and Chronic Tinnitus,” Laryngoscope, vol. 113, no. 3, pp. 427–431, Mar. 2003, doi: https://doi.org/10.1097/00005537-200303000-00007
P. Adjamian, D. A. Hall, A. R. Palmer, T. W. Allan, D. R. M. Langers, “Neuroanatomical abnormalities in chronic tinnitus in the human brain,” Neurosci. Biobehav. Rev., vol. 45, pp. 119–133, Sep. 2014, doi: https://doi.org/10.1016/j.neubiorev.2014.05.013
H. Guest, K. J. Munro, C. J. Plack, “Tinnitus with a normal audiogram: Role of high-frequency sensitivity and reanalysis of brainstem-response measures to avoid audiometric over-matching,” Hear. Res., vol. 356, pp. 116-117, Dec. 2017, doi: https://doi.org/10.1016%2Fj.heares.2017.10.002
K. Demeester, A. van Wieringen, J. Hendrickx, V. Topsakal, et al., “Prevalence of tinnitus and audiometric shape,” B-ENT, vol. 3, suppl. 7, pp. 37–49, 2007. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/18225607/
P. Simonetti, J. Oiticica, “Tinnitus Neural Mechanisms and Structural Changes in the Brain: The Contribution of Neuroimaging Research,” Int. Arch. Otorhinolaryngol., vol. 19, no. 3, pp. 259–265, 2015, doi: https://doi.org/10.1055%2Fs-0035-1548671
B. Satar, O Kapkin, Y. Ozkaptan, “Evaluation of cochlear function in patients with normal hearing and tinnitus: a distortion product otoacoustic emission study,” Kulak Burun Bogaz Ihtis. Derg., vol. 10, no. 5, pp. 177–182, 2003. [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/12970589/
R. M. Lewis, K. N. Jahn, A. Parthasarathy, W. B. Goedicke, D. B. Polley, “Audiometric Predictors of Bothersome Tinnitus in a Large Clinical Cohort of Adults With Sensorineural Hearing Loss,” Otol. Neurotol., vol. 41, no. 4, pp. e414–e421, Apr. 2020, doi: https://doi.org/10.1097/mao.0000000000002568
T. G. Sanchez, Í. R. T. de Medeiros, C. P. D. Levy, J. R. O. Ramalho, R. F. Bento, “Tinnitus in normally hearing patients: clinical aspects and repercussions,” Braz. J. Otorhinolaryngol., vol. 71, no. 4, pp. 427–431, Jul. 2005, doi: https://doi.org/10.1016/s1808-8694(15)31194-0
A. R. Møller, “Sensorineural Tinnitus: Its Pathology and Probable Therapies,” Int. J. Otolaryngol., vol. 2016, art. no. 2830157, Feb. 2016, doi: https://doi.org/10.1155/2016/2830157
B. Hofmeier, S. Wolpert, E. S. Aldamer, M. Walter, et al., “Reduced sound-evoked and resting-state BOLD fMRI connectivity in tinnitus,” NeuroImage Clin., vol. 20, pp. 637–649, 2018, doi: https://doi.org/10.1016%2Fj.nicl.2018.08.029
G. Buzsáki, N. Logothetis, W. Singer, “Scaling Brain Size, Keeping Timing: Evolutionary Preservation of Brain Rhythms,” Neuron, vol. 80, no. 3, pp. 751–764, Oct. 2013, doi: https://doi.org/10.1016/j.neuron.2013.10.002
H. Ashton, K. Reid, R. Marsh, I. Johnson, K. Alter, T. Griffiths, “High frequency localised “hot spots” in temporal lobes of patients with intractable tinnitus: a quantitative electroencephalographic (QEEG) study,” Neurosci. Lett., vol. 426, no. 1, pp. 23–28, Oct. 2007, doi: https://doi.org/10.1016/j.neulet.2007.08.034
P. Vianney-Rodrigues, O. D. Iancu, J. P. Welsh, “Gamma oscillations in the auditory cortex of awake rats,” Eur. J. Neurosci., vol. 33, no. 1, pp. 119–129, Nov. 2011, doi: https://doi.org/10.1111%2Fj.1460-9568.2010.07487.x
S. Steinmann, G. Leicht, M. Ertl, C. Andreou, et al., “Conscious auditory perception related to long-range synchrony of gamma oscillations,” NeuroImage, vol. 100, pp. 435–443, Oct. 2014, doi: https://doi.org/10.1016/j.neuroimage.2014.06.012
M. N. O’connell, A. Barczak, D. Ross, T. McGinnis, C. E. Schroeder, P. Lakatos, “Multi-Scale Entrainment of Coupled Neuronal Oscillations in Primary Auditory Cortex,” Front. Hum. Neurosci., vol. 9, art. no. 655, 2015, doi: https://doi.org/10.3389/fnhum.2015.00655
E. Houdayer, R. Teggi, S. Velikova, J. J. Gonzalez-Rosa, M. Bussi, G. Comi, L. Leocani, “Involvement of cortico-subcortical circuits in normoacousic chronic tinnitus: A source localization EEG study,” Clinical Neurophysiology., vol. 126, no. 12, pp. 2356–2365, Dec. 2015, doi: https://doi.org/10.1016/j.clinph.2015.01.027
D. De Ridder, E. van der Loo, S. Vanneste, S. Gais, et al., “Theta-gamma dysrhythmia and auditory phantom perception,” J. Neurosurg., vol. 114, no. 4, pp. 912–921, Apr. 2011, doi: https://doi.org/10.3171/2010.11.jns10335
S. Vanneste, J. J. Song, D. De Ridder, “Thalamocortical dysrhythmia detected by machine learning,” Nat. Commun., vol. 9, art. no. 1103, Mar. 2018, doi: https://doi.org/10.1038/s41467-018-02820-0
I. Adamchic, B. Langguth, C. Hauptmann, P. A. Tass, “Abnormal cross-frequency coupling in the tinnitus network,” Front. Neurosci., vol. 8, art. no. 284, Sep. 2014, doi: https://doi.org/10.3389%2Ffnins.2014.00284
J. Campbell, C. Bean, A. LaBrec, “Normal Hearing Young Adults with Mild Tinnitus: Reduced Inhibition as Measured Through Sensory Gatin,” Audiol. Res., vol. 8, no. 2, art. no. 214, Oct. 2018, doi: https://doi.org/10.4081%2Faudiores.2018.214
A. Asadpour, M. Jahed, S. Mahmoudian, “Brain Waves Evaluation of Sound Therapy in Chronic Subjective Tinnitus Cases Using Wavelet Decomposition,” Front. Integr. Neurosci., vol. 12, art. no. 38, Sep. 2018, doi: https://doi.org/10.3389%2Ffnint.2018.00038
F. Mohagheghian, B. Makkiabadi, H. Jalilvand, H. Khajehpoor, N. Samadzadehaghdam, E. Eqlimi, M. R. Deevband, “Computer-aided tinnitus detection based on brain network analysis of EEG functional connectivity,” J. Biomed. Phys. Eng., vol. 9, no. 6, pp. 687-698, Dec. 2019, doi: https://doi.org/10.31661%2Fjbpe.v0i0.937
M. J. C. van den Berge, R. H. Free, R. Arnold, E. de Kleine, R. Hofman, J. M. C. van Dijk, P. van Dijk, “Cluster analysis to identify possible subgroups in tinnitus patients,” Front. Neurol., vol. 8, art. no.115, Apr. 2017, doi: https://doi.org/10.3389/fneur.2017.00115
P. J. Sanders, Z. D. Doborjeh, M. G. Doborjeh, N. K. Kasabov, G. D. Searchfield, “Prediction of Acoustic Residual Inhibition of Tinnitus Using a Brain-Inspired Spiking Neural Network Model,” Brain Sci., vol. 11, no. 1, art. no. 52, Jan. 2021, doi: https://doi.org/10.3390/brainsci11010052
D. Ibarra-Zarate, L. M. Alonso-Valerdi, “Acoustic therapies for tinnitus: The basis and the electroencephalographic evaluation,” Biomed. Signal Process. Control, vol. 59, art. no. 101900, May 2020, doi: https://doi.org/10.1016/j.bspc.2020.101900
S. J. Morrison, Statistics for engineers: An introduction. Chichester: John Wiley & Sons, 2009, pp. 143. [Online]. Available: https://vdoc.pub/documents/statistics-for-engineers-an-introduction-56hhpsom9720
D. M. Lane, D. Scott, M. Hebl, R. Guerra, D. Osherson, H. Zimmer, Introduction to statistics. Houston, Texas, United States: David Lane, 2017, pp. 692. [Online]. Available: https://onlinestatbook.com/Online_Statistics_Education.pdf
R. Shanmugam, R. Chattamvelli, “Skewness and Kurtosis,” in: Statistics for Scientists and Engineers, R. Shanmugam, R. Chattamvelli, Eds. United States of America: John Wiley and Sons, Inc., 2015, ch. 4, pp. 89–110, doi: https://doi.org/10.1002/9781119047063.ch4
P. Stoica, R. Moses, Spectral analysis of signals. United States of America: Prentice Hall, 2005, pp. 452.
Y. Lei, Intelligent Fault Diagnosis and Remaining Useful Life Prediction of Rotating Machinery. United States of America: Butterworth-Heinemann, 2017, pp. 366, doi: https://doi.org/10.1016/C2016-0-00367-4
L. Si, Z. Wang, C. Tan, X. Liu, “Vibration-Based Signal Analysis for Shearer Cutting Status Recognition Based on Local Mean Decomposition and Fuzzy C-Means Clustering,” Appl. Sci., vol. 7, no. 2, art. no. 164, Feb. 2017, doi: https://doi.org/10.3390/app7020164
C. Altin, E. Orhan, “Comparison of Different Time and Frequency Domain Feature Extraction Methods on Elbow Gesture’s EMG,” Eur. J. Interdiscip. Stud., vol. 2, no. 3, pp. 35–44, Aug. 2016, doi: http://dx.doi.org/10.26417/ejis.v2i3.35-44
H. W. Lilliefors, “On the Kolmogorov-Smimov Tests for Normality with Mean and Variance Unknown,” J. Am. Stat. Assoc., vol. 62, no. 318, pp. 399–402, 1967, doi: https://doi.org/10.2307/2283970
D. D. Wackerly, W. Mendenhall, R. L. Scheaffer, Estadística matemática con aplicaciones, 7th ed. México: CENGAGE Learning, 2008, pp. 911.
Descargas
Publicado
Cómo citar
Número
Sección
Licencia
Derechos de autor 2023 Revista Mexicana de Ingenieria Biomedica

Esta obra está bajo una licencia internacional Creative Commons Atribución-NoComercial 4.0.
Una vez que el artículo es aceptado para su publicación en la RMIB, se les solicitará al autor principal o de correspondencia que revisen y firman las cartas de cesión de derechos correspondientes para llevar a cabo la autorización para la publicación del artículo. En dicho documento se autoriza a la RMIB a publicar, en cualquier medio sin limitaciones y sin ningún costo. Los autores pueden reutilizar partes del artículo en otros documentos y reproducir parte o la totalidad para su uso personal siempre que se haga referencia bibliográfica al RMIB. No obstante, todo tipo de publicación fuera de las publicaciones académicas del autor correspondiente o para otro tipo de trabajos derivados y publicados necesitaran de un permiso escrito de la RMIB.